For decades, reconstructive surgery has been a beacon of hope. It’s the art and science of rebuilding—after trauma, cancer, or birth differences. But let’s be honest, it’s often come with trade-offs. Harvesting tissue from a patient’s thigh or back is a major ordeal. Synthetic implants can feel… foreign. The goal has always been restoration, but the methods, well, they sometimes left their own scars.
That’s where regenerative medicine swerves in, not to replace the surgeon’s skill, but to supercharge it. Imagine not just moving tissue from point A to point B, but actually convincing the body to grow its own new, living tissue. That’s the powerful intersection we’re exploring today. It’s a shift from reconstruction to true regeneration.
From Patching to Re-Growing: A Core Philosophy Shift
Traditional reconstructive surgery is, in a way, a brilliant workaround. It’s like a master carpenter using the best available wood to repair a cherished piece of furniture. Regenerative medicine asks: “What if we could get the original wood to grow back?”
This isn’t science fiction anymore. It’s a practical convergence focused on harnessing the body’s innate—but often dormant—healing capabilities. The surgeon’s role evolves. They become architects of the biological environment, creating the perfect conditions for the body to heal itself.
The Toolkit: What’s Actually in the Regenerative Arsenal?
So, what does this look like in the OR? It’s not one magic bullet. It’s a suite of strategies, often used in combination. Here’s the deal with the key players:
- Stem Cells: The body’s raw material. These aren’t just controversial embryonic cells—we’re talking about adult stem cells, like those from your own fat (adipose-derived) or bone marrow. They’re like cellular directors, signaling local tissues to repair and reduce inflammation.
- Growth Factors & PRP (Platelet-Rich Plasma): Think of these as the fertilizer. By concentrating the proteins and factors from your own blood that signal healing, surgeons can create a potent cocktail to accelerate recovery and improve graft survival.
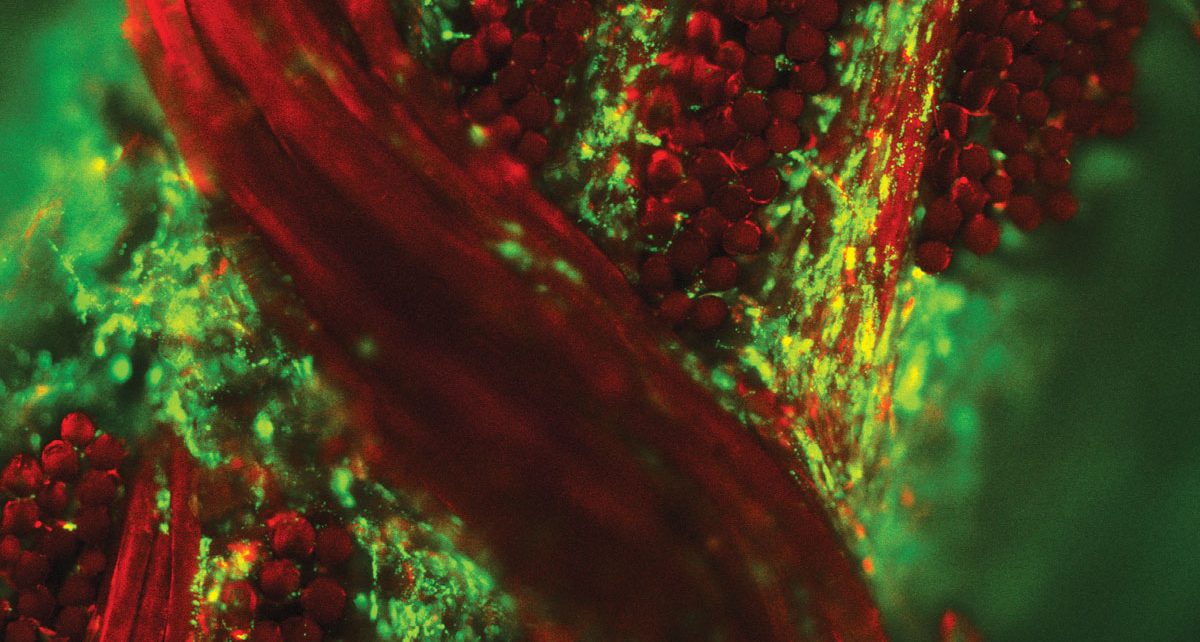
- Biologic Scaffolds: These are the temporary frameworks. Made from animal or donor tissues stripped of cells, these 3D structures act like a “guide rail” for your own cells to migrate into and rebuild. It’s like providing a trellis for a climbing rose.
- Fat Grafting & Tissue Engineering: This is where it gets really hands-on. We’re not just transplanting fat for volume anymore. By enriching fat with stem cells and growth factors (creating so-called cell-assisted lipotransfer), the fat is more likely to survive and integrate, fighting the unpredictability that’s long plagued the procedure.
Where the Rubber Meets the Road: Real-World Applications
Okay, theory is great. But where is this actually changing lives right now? The impact is profound in a few key areas.
Breast Reconstruction: A Softer, More Natural Path
Post-mastectomy, women have faced a tough choice: implants or autologous tissue flaps (that major muscle harvest we mentioned). Regenerative techniques are offering a third way. Using biologic scaffolds seeded with the patient’s own cells, surgeons can now help the body regenerate a new, soft tissue framework. The result? A reconstruction that feels more natural, ages with the patient, and avoids the complications of foreign material. It’s a quieter, more elegant solution.
Complex Wound Healing: Closing the “Unclosable”
Chronic wounds—from diabetes, radiation injury, or massive trauma—are a nightmare. They stall, they get infected. Here, regenerative medicine acts as a jump-start. Applying stem cell-rich concentrates or layered scaffolds to these wounds delivers a direct shot of healing signals. It tells the stagnant wound bed: “Hey, it’s time to rebuild.” The outcomes? Faster closure, better quality skin, and, crucially, less scarring.
Craniofacial and Burn Reconstruction: Restoring Form and Function
Rebuilding a nose, an ear, or a jaw after injury is incredibly complex. The goal isn’t just to look right, but to function. Cartilage needs to be flexible, bone needs to be strong. Researchers are now 3D-printing biocompatible scaffolds in the exact shape of the missing anatomy, then seeding them with the patient’s cells. Over time, the scaffold dissolves, leaving behind living, functional tissue. For burn victims, spraying a patient’s own stem cells onto a wound can dramatically improve healing and reduce contractures.
The Challenges: It’s Not All Smooth Sailing (Yet)
Let’s not get carried away. This field is still, in many ways, in its adolescence. The hype can outpace the reality. Regulation is a tangled web—the FDA carefully distinguishes between minimally manipulated tissues (like your own fat moved to your breast) and more complex biologic drugs. Cost is a huge barrier; these technologies are expensive. And perhaps the biggest hurdle? Consistency.
Biology is messy. Getting the same reliable, reproducible result every single time is the holy grail we’re still chasing. It’s why much of this work happens in major academic centers as part of clinical trials.
| Current Approach | Regenerative-Enhanced Approach | Patient Impact |
| Autologous tissue flap | Cell-enriched fat grafting + scaffold | Less donor site morbidity, more natural feel |
| Skin grafts for burns | Stem cell sprays or cultured skin substitutes | Improved healing, less scarring, more flexibility |
| Bone grafts from hip | 3D-printed bioactive bone scaffold | Custom shape, no second surgical site, better integration |
The Future Is Integration, Not Replacement
So, what’s next? The most exciting vision isn’t a robot doing surgery with stem cells. It’s the surgeon, with a deeper understanding of molecular biology, wielding a new set of tools. The OR of the future might have a “biologics lab” right next door, preparing personalized cell therapies while the operation is underway.
We’re moving towards personalized regenerative protocols. Your unique biology could dictate the precise cocktail of cells and scaffolds needed for your optimal healing. The line between healer and gardener is blurring in the best possible way.
The intersection of these two fields is, ultimately, about hope. A quieter, more elegant kind of hope. It’s the hope for a repair that feels less like a patch and more like a second chance. The body remembers how to be whole. Modern medicine is finally learning how to listen.